Beyond Arson: A Closer Look at Pyromania Disorder
Beyond Arson: A Closer Look at Pyromania Disorder
Explore the complexities of pyromania, a misunderstood psychiatric disorder, and uncover the latest in its diagnosis and compassionate treatment approaches.
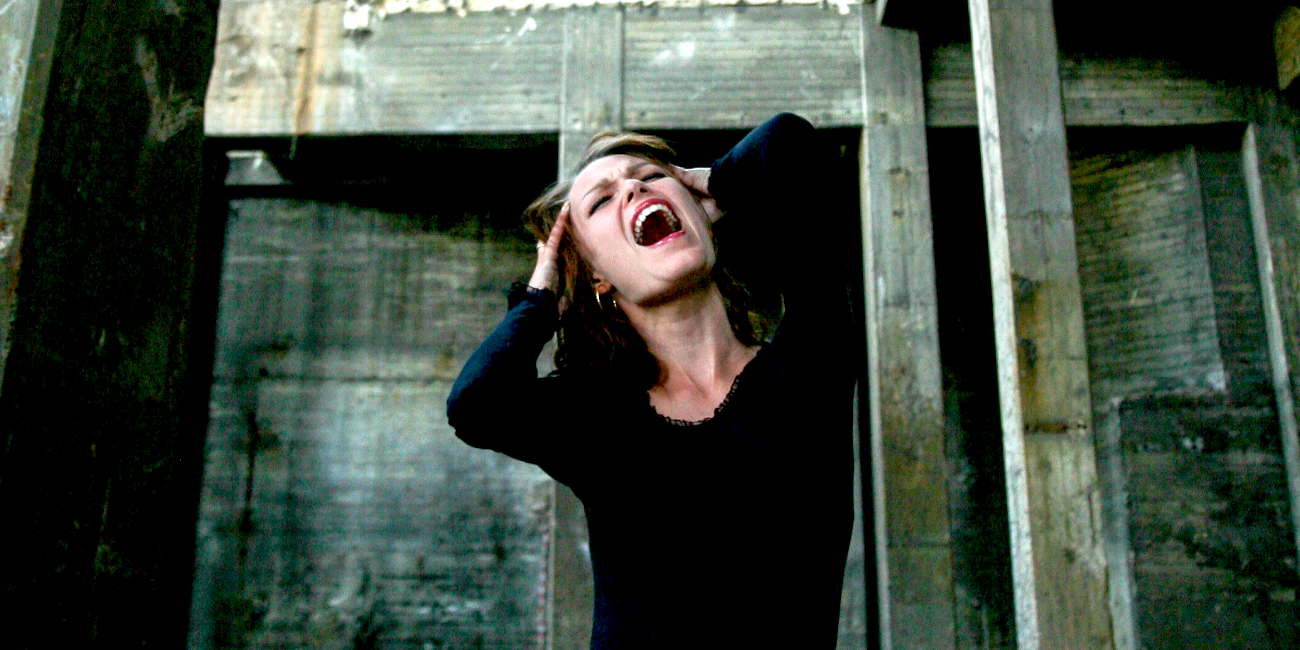
Pyromania is a rare psychiatric disorder characterized by an impulse control disorder that involves a fascination with, interest in, or attraction to fire and fire-starting activities. Individuals with pyromania experience an emotional buildup or arousal before setting a fire and relief or pleasure upon setting it or witnessing the ensuing blaze. These behaviors are not motivated by monetary gain, ideological beliefs, a desire to conceal criminal activity, expressions of sociopolitical ideology, anger, or vengeance. They are also not the result of delusional thinking, hallucinations, impaired judgment due to substance abuse, or a manic episode.
People presenting with pyromania are often described as obsessed with fire and fire-setting. This preoccupation can manifest in various ways, such as a compulsion to set fires or an intense interest in fire-related activities and paraphernalia. They may make considerable preparations for starting fires and derive gratification from the act itself as well as the associated stimuli (e.g., sights, sounds, smells). Moreover, these individuals may experience tension or affective arousal before the act and relief or pleasure afterward.
Pyromania is distinguished from other fire-setting behaviors by the emotional states associated with fire setting. Unlike arsonists, individuals with pyromania do not set fires for monetary gain, to express anger, or for any other intentional purpose. The behavior is impulsive and repetitive, with fires set more for instant gratification rather than for any external rewards.
Diagnostic Criteria
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), outlines specific criteria for diagnosing pyromania. According to DSM-5-TR, pyromania is characterized by deliberate and purposeful fire setting on multiple occasions. Individuals diagnosed with pyromania experience feelings of tension or emotional arousal before the act and show a fascination with, interest in, or attraction to fire and its situational contexts (e.g., paraphernalia, uses, consequences). There is pleasure, gratification, or relief when setting fires or witnessing or participating in their aftermath. The fire setting is not done for monetary gain, as an expression of ideological beliefs, to conceal criminal activity, to express anger or vengeance, as a response to a delusion or hallucination, or as a result of impaired judgment (e.g., due to dementia, substance intoxication).
The DSM-5-TR also stipulates that the fire setting cannot be better accounted for by conduct disorder, a manic episode, or antisocial personality disorder. Moreover, the behavior must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning for the individual.
The exact cause of pyromania is poorly understood, but it is believed to involve a combination of genetic, environmental, and psychological factors. The rarity of the disorder has made it difficult for researchers to study it extensively. As a result, much of the literature on pyromania is based on case studies or small sample sizes. However, some research suggests that individuals with pyromania may have abnormalities in brain areas responsible for impulse control and judgment.
It is important to note that the diagnosis of pyromania is rare, and the disorder is often underdiagnosed or misdiagnosed. When evaluating for pyromania, clinicians must carefully differentiate the disorder from more common issues such as conduct disorder in adolescents or arson for criminal purposes.
Comorbidities
Pyromania, a rare impulse control disorder characterized by an irresistible urge to start fires, often has comorbid conditions that complicate its clinical picture. These comorbidities can range from other impulse control disorders to various affective and anxiety disorders.
One common comorbidity is substance use disorders. Individuals with pyromania may also abuse alcohol or drugs, potentially as a means of self-medication or as part of a broader pattern of impulsivity (Grant & Kim, 2003). Mood disorders, particularly depression and bipolar disorder, have also been associated with pyromania. The link between mood dysregulation and impulse control disorders suggests a shared vulnerability or a causal relationship where the distress from the mood disorder enhances the risk for impulsive and destructive behaviors like fire-setting.
Anxiety disorders, including post-traumatic stress disorder (PTSD), have been noted in some cases. Traumatic experiences, particularly those involving fire or violence, can manifest later as pyromania, possibly as a maladaptive coping mechanism or a re-enactment of trauma (Dell’Osso et al., 2010). Additionally, personality disorders, incredibly antisocial personality disorder, are frequently cited as comorbid with pyromania, with both disorders involving a disregard for the safety of oneself or others (Grant & Kim, 2003).
Attention-deficit/hyperactivity disorder (ADHD) is another condition that can co-occur, with impulsivity being a core feature of both disorders. This impulsivity can lead to many problematic behaviors, including the compulsion to set fires (Silva et al., 2008).
These comorbidities pose challenges for treatment, as they may influence the course of the disorder and its responsiveness to treatment. Therapeutic approaches need to be comprehensive and tailored to address not only the pyromania but also the accompanying psychiatric conditions.
Treatment and Interventions
The treatment and interventions for pyromania are multimodal, often involving a combination of psychotherapy, behavioral modifications, and medication. However, there is no standard treatment regimen due to the rarity of the disorder. Cognitive-behavioral therapy (CBT) is commonly employed to help individuals with pyromania identify and modify problematic thought patterns and behaviors related to fire setting (Grant & Kim, 2003). Through CBT, individuals can learn coping strategies to resist impulses to set fires and better manage the emotions that contribute to their fire-setting behaviors.
Behavioral interventions, such as aversion therapy and covert sensitization, have also been used in the treatment of pyromania. Aversion therapy involves pairing the act of setting a fire with a negative consequence or unpleasant stimulus. At the same time, covert sensitization involves individuals imagining adverse outcomes from a fire setting (Kolko, 1985). These interventions aim to reduce the pleasurable associations with fire setting.
In terms of pharmacotherapy, there is some evidence suggesting that selective serotonin reuptake inhibitors (SSRIs) can be helpful, particularly if the individual with pyromania also has comorbid conditions such as obsessive-compulsive disorder (OCD) (Grant, 2005). SSRIs are believed to help by reducing the impulsive behaviors characteristic of pyromania. However, more research is needed to establish the efficacy and safety of SSRIs for this specific disorder.
Family therapy may also play a role in the treatment of pyromania, especially in juvenile cases. Involving the family can help in creating a supportive environment that is conducive to recovery. This approach can also address family dynamics contributing to the individual's fire-setting behavior (Kolko, 1996).
It is crucial to note that treatment for pyromania must be highly individualized, taking into account the severity of the disorder, the presence of comorbid conditions, and the specific characteristics of the individual. Since the evidence base for the treatment of pyromania is not as robust as for other psychiatric disorders, clinicians often rely on their clinical experience and judgment when developing a treatment plan.
Summary
Pyromania is a challenging and often misunderstood disorder. Historically, individuals with a penchant for fire settings were harshly judged and often treated as criminals rather than as people suffering from a psychiatric disorder. Over time, however, perspectives have shifted, recognizing pyromania as a mental health condition that requires understanding, appropriate intervention, and compassion. The evolution of diagnostic criteria in the DSM has contributed to a more nuanced understanding of the disorder, allowing for better differentiation from criminal arson (American Psychiatric Association, 2023).
Despite these advances, diagnosing pyromania remains complex. Its rarity contributes to less empirical knowledge compared to more prevalent disorders, and its symptoms can overlap with other psychiatric conditions, leading to underdiagnosis or misdiagnosis. Moreover, the clandestine nature of fire setting and the social stigma associated with it can lead individuals to hide their behavior, thus delaying or avoiding treatment altogether (Grant & Kim, 2003).
The interpersonal consequences for those with pyromania can be severe, often leading to relationship disruptions. The incomprehension and fear that a fire setting arouses in others can result in social isolation for the individual with pyromania. This, combined with the inherent dangers of the behavior, can significantly strain family, occupational, and social relationships (Kolko, 1985).
The impact on identity and confidence for those with pyromania is also notable. The compulsion to set fires can become a central aspect of a person's identity, overshadowing other characteristics and contributions. The shame and guilt associated with the behavior, coupled with the fear of legal consequences, can undermine self-esteem and exacerbate feelings of alienation (Laberge & Drapeau, 1999; Borrell-Carrió et al., 2004).
Understanding and treating pyromania requires an empathetic and multidisciplinary approach. Clinicians and researchers continue to advocate for more comprehensive studies to enhance treatment strategies and societal responses to this disorder. The movement towards a more inclusive and compassionate view of pyromania reflects broader changes in how society perceives and responds to mental health challenges, emphasizing the importance of dignity, support, and evidence-based care for all individuals.
References
Grant, J. E. (2005). Impulse control disorders: A clinician's guide to understanding and treating behavioral addictions. Norton & Company.
Grant, J. E., & Kim, S. W. (2007). Clinical characteristics and psychiatric comorbidity of pyromania. Journal of Clinical Psychiatry, 68(11), 1717-1722.
Kolko, D. J. (1985). The assessment and treatment of children who abuse fire: Preliminary data. American Journal of Orthopsychiatry, 55(1), 73–85.
Kolko, D. J. (1996). Individual cognitive-behavioral treatment and family therapy for physically abused children and their offending parents: A comparison of clinical outcomes. Child Maltreatment, 1(4), 322–342.
Laberge, L., & Drapeau, M. (1999). A biopsychosocial model of arson. Aggression and Violent Behavior, 4(1), 55-69.
Borrell-Carrió, F., Suchman, A. L., & Epstein, R. M. (2004). The Biopsychosocial Model 25 Years Later: Principles, Practice, and Scientific Inquiry. Annals of Family Medicine, 2(6), 576-582.
Dell’Osso, L., Berlin, H. A., Serati, M., & Altamura, A. C. (2010). Neuropsychobiological aspects, comorbidity patterns and dimensional models in borderline personality disorder. Neuropsychobiology, 61(4), 169-79.
Grant, J. E., & Kim, S. W. (2003). Comorbidity of impulse control disorders in pathological gamblers. Acta Psychiatrica Scandinavica, 108(3), 203–207.
Silva, D., Storch, E. A., & Geffken, G. R. (2008). ADHD and the rise in stimulant use among children. Harvard Review of Psychiatry, 16(3), 151-166.