Transient Turmoil: Understanding Brief Psychotic Disorder
Transient Turmoil: Understanding Brief Psychotic Disorder
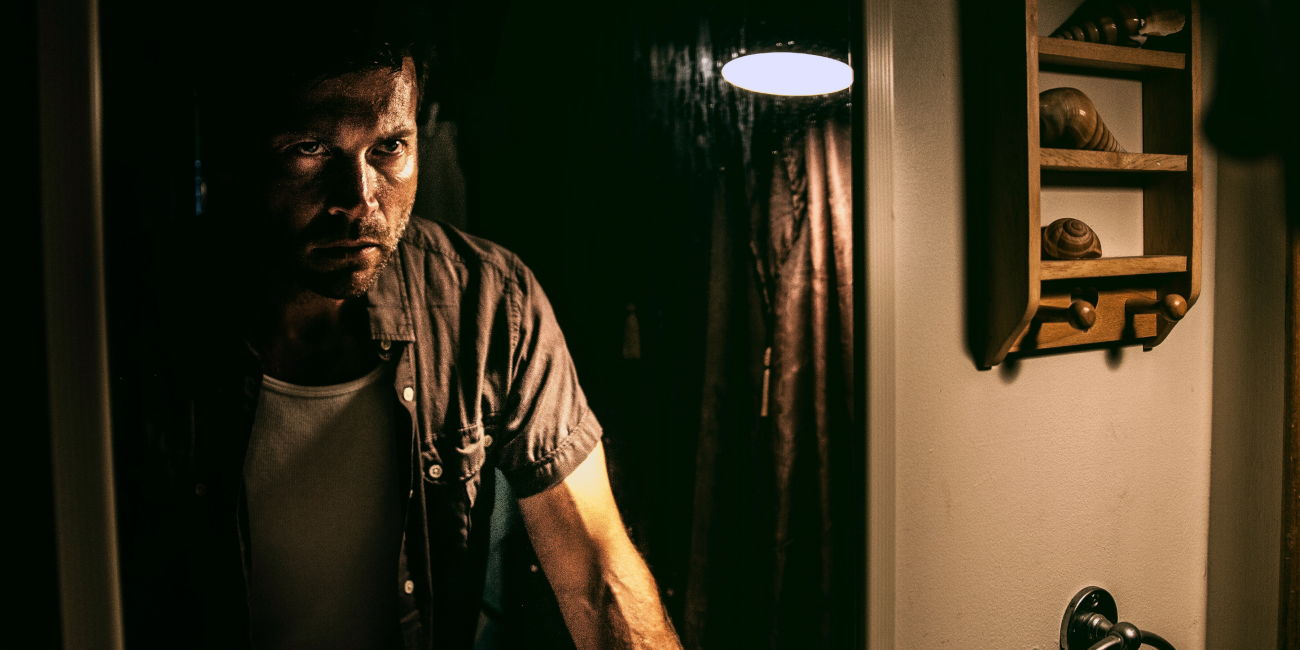
Venturing into the enigma of Brief Psychotic Disorder, I unearth the profound impact of transient mental disturbances and the glimmer of hope modern research offers. Explore the complexities, challenges, and the promising road to recovery for those affected.
Brief Psychotic Disorder is a psychiatric condition characterized by sudden onset psychotic symptoms, such as hallucinations (perceiving things that are not there), delusions (firmly held false beliefs), or disorganized speech. For a diagnosis to be made, the symptoms must last for at least one day but less than one month, after which the individual fully returns to their baseline level of functioning. The cause of this disorder can vary, but it often follows significant stress or trauma. It is distinct from other psychotic disorders in duration and the complete return to the baseline function. It also differs from mood disorders with psychotic features because mood symptoms do not primarily characterize it.
Factors that might contribute to the onset of this disorder include significant stress, postpartum onset (with symptoms starting within four weeks after giving birth), or potential links to physical illnesses or the use of certain medications or drugs. It is worth noting that the prognosis for Brief Psychotic Disorder is typically good, with many individuals never experiencing another episode again. However, diagnosing and treating the condition promptly is crucial to ensure that symptoms are managed appropriately.
Diagnostic Criteria
A brief Psychotic Disorder is like a sudden, short-lived storm of confusion and unusual experiences in someone's mind. A significant stressful event can trigger it, but not always. Some new moms might also experience it after giving birth. The good news is, unlike other conditions, people usually get back to their usual selves after this brief episode. The diagnostic criteria for Brief Psychotic Disorder, as outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by the American Psychiatric Association (2013), are as follows.
A person with Brief Psychotic Disorder may grapple with unique beliefs, envision or hear nonexistent things, struggle with coherent speech, or exhibit peculiar behaviors, even reaching states of near-immobility. These intense symptoms emerge rapidly, persisting for a day or more but dissipating within a month, allowing the individual to revert to their typical demeanor. Crucially, these manifestations aren't attributed to mood disorders, enduring psychotic conditions, substances, medications, or other health issues.
Sometimes, the symptoms of Brief Psychotic Disorder manifest following a highly stressful event, while at other times, they can emerge without any noticeable precipitating stressors. Additionally, in certain instances, these symptoms initiate during pregnancy or within a month postpartum
The Impacts
Brief Psychotic Disorder, while short-lived, can have significant impacts on an individual's life, both in immediate consequences and potential longer-term implications. Let us delve into the effects and refer to relevant psychology research:
- Immediate Disruption: Individuals with Brief Psychotic Disorder may find their daily life, work, relationships, and routine severely disrupted during the episode. They might be unable to carry out everyday tasks or responsibilities due to the intensity of the symptoms.
- Emotional and Psychological Impact: Experiencing symptoms like hallucinations and delusions can be terrifying and confusing. People may feel isolated or ashamed, potentially leading to depressive symptoms or heightened anxiety once the psychotic episode resolves (Ran et al., 2015).
- Social Impact: The unpredictable nature of the disorder can strain relationships with friends and family who might not understand what is happening. Social withdrawal or stigmatization might further isolate the individual (Hanzawa et al., 2011).
- Economic Consequences: Sudden disruptions in the ability to work or perform regular tasks can lead to financial difficulties or job loss. There is also the cost associated with potential hospitalization or medical care.
- Risk of Recurrence: Although many individuals with Brief Psychotic Disorder may never experience another episode, some may have recurrences, leading to anxiety about when and if another episode might occur (Susser et al., 1994).
- Potential for Future Mental Health Concerns: Some individuals might develop more prolonged psychotic disorders, mood disorders, or other mental health conditions after an episode of Brief Psychotic Disorder (Kelleher & Cannon, 2011).
The unexpected onset of Brief Psychotic Disorder is particularly unsettling, primarily because it often surfaces without any preceding signs or history of psychotic behavior. This abrupt emergence can be likened to a clear sky suddenly overtaken by a storm. For the person experiencing it, the world shifts without warning: beliefs become distorted, perceptions might not align with reality, and their speech or behavior may become disorganized. This sudden change can be deeply distressing, leading to fear, isolation, and confusion. Moreover, the transformation can be equally jarring for their family, friends, and colleagues. They might struggle to understand what is happening, potentially leading to misinterpretations, fear, or stigmatization. Research has shown that sudden onset mental health disorders can be incredibly challenging because they disrupt the established equilibrium of one's life, leading to significant emotional, social, and sometimes economic upheavals (Malla et al., 2005). Furthermore, the lack of prior history means there is no roadmap for the affected individual and their loved ones, leaving them unprepared to navigate the crisis and often at a loss for how to offer or seek appropriate support (Perry et al., 2007).
The Etiology (Origins and Causes)
The etiology or causes of Brief Psychotic Disorder are diverse and not fully understood. Several factors have been proposed based on the available research literature:
- Stress and Trauma: A significant body of research suggests that acute stress or traumatic events can precipitate the onset of Brief Psychotic Disorder. This kind of response to extreme stress has led to the term "brief reactive psychosis" in some cases (Susser et al., 1994).
- Biological Factors: There might be some neurobiological predispositions. Abnormalities in brain structure, function, or neurotransmitter systems, particularly dopamine, have been implicated in various psychotic disorders (Howes & Kapur, 2009).
- Genetic Predisposition: While there is no direct evidence that Brief Psychotic Disorder is hereditary, having family members with psychiatric disorders might increase the risk (Kendler et al., 1998).
- Postpartum Onset: Changes in hormones, stress related to childbirth, and the physiological stresses of pregnancy and delivery have been associated with the postpartum onset of the disorder (Brockington, 2004).
- Substance Use: The use or withdrawal from certain substances, including alcohol, cannabis, and hallucinogens, can contribute to transient psychotic symptoms (Thirthalli & Benegal, 2006).
- Medical Conditions: Some medical conditions that affect the brain, such as epilepsy or certain endocrine disorders, might precipitate brief psychotic symptoms (Mendez et al., 2008).
- Cultural Factors: Some behaviors or beliefs considered "psychotic" in one culture might be deemed normal in another, so cultural context is vital when diagnosing (Bhugra & Bhui, 2000).
While various factors may contribute to the onset of Brief Psychotic Disorder, the exact cause often remains elusive. Multiple factors might also interact, making pinpointing a singular cause for any individual case challenging.
The etiology of Brief Psychotic Disorder is challenging to pin down because of its multifaceted nature. The very essence of the disorder, being transient and short-lived, makes it difficult for researchers to study it systematically compared to more chronic conditions. Additionally, a complex interplay of biological, psychological, social, and environmental factors could potentially contribute to its onset. For instance, while one individual might develop symptoms following an acute stressor, another might show symptoms without any discernible trigger. This variability makes it challenging to identify consistent causal factors across individuals. Furthermore, the nature of psychotic symptoms means that gathering accurate and comprehensive data from affected individuals, especially during an episode, can be intricate.
All these complexities, combined with potential genetic predispositions and the influence of substances or medical conditions, have left gaps in our understanding of the disorder's precise origins despite continuous advancements in psychiatric research.
Comorbidities
Brief Psychotic Disorder has several comorbidities that can arise either as predisposing factors, consequences, or as conditions that coexist with it:
- Mood Disorders: Particularly Major Depressive Disorder and Bipolar Disorder. Some individuals may experience depressive symptoms or manic episodes alongside or following their brief psychotic episodes (Mojtabai, 2006).
- Anxiety Disorders: The experience of psychosis can be terrifying, and some individuals may develop anxiety disorders, such as Generalized Anxiety Disorder or Post-Traumatic Stress Disorder, as a result of the trauma associated with their psychotic episode (Melle et al., 2004).
- Substance Use Disorders: Substance abuse, particularly of hallucinogens, cannabis, or stimulants, can both trigger brief psychotic symptoms and become a subsequent issue. Some individuals might use substances to cope with the memory or aftermath of a psychotic episode (Arndt et al., 1991).
- Postpartum Psychiatric Disorders: For women, the postpartum period can be associated with various psychiatric conditions, including Postpartum Depression and Postpartum Psychosis. Brief Psychotic Disorder can occur in this period and may be intertwined with other postpartum conditions (Brockington, 2004).
- Personality Disorders: Some studies suggest that individuals with certain personality disorders, such as Borderline Personality Disorder, might be more susceptible to transient episodes of psychosis (Riordan et al., 1996).
- Medical Conditions: Some medical disorders, especially those affecting the brain or hormonal balance (e.g., endocrine disorders, neurological conditions), might coexist with or precipitate brief psychotic episodes (Mendez et al., 2008).
- Dissociative Disorders: There can be an overlap between symptoms of Brief Psychotic Disorder and dissociative disorders, especially in response to trauma (Spiegel et al., 2011).
There are several reasons why these comorbidities present challenges. Similar or overlapping symptoms in different disorders make it challenging to determine the primary cause. For instance, psychosis can be a symptom of schizophrenia and bipolar disorder. Distinguishing between transient psychosis, like in Brief Psychotic Disorder, and longer-lasting psychosis found in other conditions requires careful evaluation (Maj, 2007).
One disorder often masks the symptoms of the other. For example, if someone is using substances, it might be initially presumed that the psychotic symptoms are purely substance-induced, potentially overlooking an underlying Brief Psychotic Disorder or vice versa (Caton et al., 2005). The presence of multiple potential disorders requires a differential diagnosis process, where the clinician must rule out one disorder after another based on symptom presentation, duration, and other factors. This process can be time-consuming and requires extensive expertise (Baldwin et al., 2005), particularly for Brief Psychotic Disorder.
Risk Factors
Brief Psychotic Disorder is a relatively less studied condition compared to other psychotic disorders like schizophrenia. However, several risk factors identified in the literature can predispose an individual to develop Brief Psychotic Disorder. Here are some of those risk factors supported by the psychological literature:
- Stress: A major or sudden stressful event can act as a trigger for Brief Psychotic Disorder. Such events might include the sudden death of a loved one, trauma, or other significant life changes (Myers et al., 1991).
- Postpartum Period: Some women may develop Brief Psychotic Disorder shortly after giving birth. This period can bring a combination of hormonal changes, sleep deprivation, and emotional adjustments, all of which can potentially contribute to the onset of the disorder (Brockington, 2004).
- Personal or Family History of Psychotic Disorders: Individuals with a personal or family history of psychotic or mood disorders may be at increased risk of developing Brief Psychotic Disorder (Mojtabai, 2006).
- Substance Use: Abuse of drugs, especially hallucinogens or stimulants, can predispose individuals to transient psychotic episodes, which might align with the criteria for Brief Psychotic Disorder (Arndt et al., 1991).
- Trauma: Exposure to traumatic events, especially recent ones, can be a risk factor for developing Brief Psychotic Disorder (Melle et al., 2004).
Case Study
Background: Lisa, a 28-year-old accountant, has always been known as a diligent worker, loving daughter, and dependable friend. She had no history of mental health disorders, and her physical health was excellent. Her family has no known history of mental illness.
Onset: A couple of weeks after the sudden death of her younger brother in a car accident, Lisa began exhibiting unusual behaviors. She often talked to herself, saying she could hear her brother calling out to her. She became convinced that he was sending her secret messages through the radio.
Symptoms: At work, Lisa's performance deteriorated rapidly. She began claiming that her computer was "alive" and that it was plotting against her. She would get startled easily, often glancing around as if she saw things others did not. Lisa became socially isolated, distancing herself from friends and family, claiming they would not "understand the messages."
Intervention: Lisa's friends noticed these changes and were deeply concerned. One of them recommended that she see a psychiatrist. The psychiatrist conducted a thorough evaluation, ruling out substance abuse and other potential medical conditions that could be causing her symptoms.
Given her recent traumatic experience and the sudden onset of her symptoms, the psychiatrist diagnosed Lisa with Brief Psychotic Disorder. The connection between the trauma of her brother's unexpected death and her symptoms became evident.
Treatment: Lisa was prescribed a short course of antipsychotic medication to manage her symptoms. She also began attending grief counseling sessions to process the trauma of losing her brother.
Outcome: Lisa's hallucinations and delusions had significantly diminished within a month. After two months, she stopped taking the antipsychotic medication under her psychiatrist's guidance. The counseling sessions helped her cope with her grief more adaptively, and she gradually returned to her previous state of well-being.
Follow-up: Six months later, Lisa returned to her regular routine, excelling at her job and rebuilding the relationships she had strained during her episode. With the support of her loved ones and her therapist's guidance, she learned to remember her brother in a way that was both honoring and healing.
This case study illustrates how Brief Psychotic Disorder can manifest after a traumatic event, and with timely intervention and support, individuals can fully recover.
Recent Psychological Research Findings
Research on Brief Psychotic Disorder has consistently highlighted the transitory nature of its symptoms and the potential factors that could trigger these episodes. A predominant theme across studies is the association between acute stress or trauma and the onset of Brief Psychotic Disorder symptoms. For instance, Susser et al. (1995) found that significant life events, especially those perceived as unfavorable, increased the risk of brief psychotic episodes.
Similarly, the postpartum period emerged as a vulnerable time for some women, with hormonal changes, sleep deprivation, and emotional adjustments being potential contributing factors (Brockington, 2004). Brief Psychotic Disorder in the postpartum context was an area of particular interest, with research indicating that the severity of episodes could vary but often resolved within weeks.
Another area of exploration was the differentiation between Brief Psychotic Disorder and other psychiatric disorders. Mojtabai (2006) emphasized distinguishing between Brief Psychotic Disorder and other conditions with psychotic features, such as schizophrenia, schizoaffective disorder, or bipolar disorder. The study found that while the brief nature of Brief Psychotic Disorder makes it distinct, overlapping symptoms could often cause diagnostic challenges, emphasizing the need for careful clinical assessment.
Substance use, particularly hallucinogens or stimulants, was another factor linked to transient psychotic episodes. Arndt et al. (1991) documented that while not all substance-induced psychosis could be categorized as Brief Psychotic Disorder, the temporal relationship between substance use and the onset of psychotic symptoms warranted scrutiny.
While Brief Psychotic Disorder is considered a distinct disorder, the potential for its episodes to progress to other psychotic disorders has also been investigated. Some findings indicated that a subset of individuals might later meet the criteria for schizophrenia or other related disorders (Keshavan et al., 2003), implying the importance of monitoring and early intervention.
Treatment and Interventions
Effective management of Brief Psychotic Disorder often involves a combination of medical, therapeutic, and environmental interventions. Here are some well-regarded methods:
- Antipsychotic Medications: These are often the first line of treatment for Brief Psychotic Disorder. Antipsychotics can help alleviate symptoms like hallucinations, delusions, and disorganized thoughts. Some commonly used antipsychotics (Marder et al., 1997; Tollefson et al., 1997) include Risperidone (Risperdal), Olanzapine (Zyprexa), Haloperidol (Haldol), Quetiapine (Seroquel), and Aripiprazole (Abilify). Typically, these are prescribed for a short duration, given the transitory nature of Brief Psychotic Disorder.
- Hospitalization: If there is a risk to oneself or others, or if symptoms are too severe to be managed in an outpatient setting, brief hospitalization can be necessary. Hospitalization ensures safety, close monitoring, and stabilization of symptoms (Kessing, 1999).
- Psychotherapy: Individual therapy can help the person make sense of the episode, develop coping strategies, and address any underlying stressors or triggers that might have contributed to the onset of the disorder.
- Cognitive Behavioral Therapy (CBT): Individual therapy can provide vital support, insights, and coping strategies. In particular, cognitive Behavioral Therapy (CBT) effectively treats symptoms and prevents relapse in psychotic disorders (Wykes et al., 2008).
- Supportive therapy: This provides emotional support, encouragement, and reassurance, helping individuals navigate the episode.
- Family Therapy: Involving the family can be crucial for support and education. Family interventions have effectively reduced relapse rates and improved outcomes for individuals with psychotic disorders (Pharoah et al., 2010).
- Stress Management: As significant stress or traumatic events can trigger episodes of Brief Psychotic Disorder, interventions that teach individuals how to manage stress effectively can be beneficial (Myin-Germeys & van Os, 2007).
- Avoidance of Substance Abuse: Substance use can exacerbate the symptoms of Brief Psychotic Disorder or even contribute to its onset. Abstaining from substance use during treatment is typically recommended (Dixon, 1999).
- Regular Medical Check-up: Since medical conditions or medication side effects can sometimes trigger Brief Psychotic Disorder, regular medical evaluations can help in early detection and appropriate adjustments.
- Community Support: Joining a support group or community program can provide the patient and their family with understanding, acceptance, and valuable insights from others who have gone through similar experiences.
It is essential to approach Brief Psychotic Disorder holistically and customize the treatment plan based on individual needs. Regular follow-ups with mental health professionals ensure the treatment remains effective and adjusts as required. Remember, most people with Brief Psychotic Disorder recover fully with appropriate treatment, but monitoring for any potential recurrence or emergence of other mental health conditions is crucial.
Implications if Untreated
Leaving Brief Psychotic Disorder untreated can have many consequences for individuals and those around them. From the literature, it becomes evident that untreated psychotic episodes, even those that are brief, can lead to several short-term and long-term complications.
First and foremost, there is an increased risk of harm without appropriate treatment. Individuals may act on delusional beliefs or hallucinations, leading to potentially harmful behaviors toward themselves or others (Wiersma et al., 1998). Such actions are often impulsive and may arise from the distorted perceptions and beliefs characteristic of psychosis.
Further, untreated Brief Psychotic Disorder can significantly impair one's ability to function in daily life. This includes disruptions in work, relationships, and general day-to-day activities (Rabinowitz et al., 2006). If not addressed, these functional impairments can result in longer-term socioeconomic consequences such as job loss, financial strain, and disrupted relationships.
Moreover, while Brief Psychotic Disorder is a transient condition with symptoms lasting between a day to a month, untreated episodes might lead to prolonged symptoms or increase the risk of recurrence (Salvatore et al., 2007). Evidence suggests that some individuals with untreated Brief Psychotic Disorder may eventually develop more chronic psychotic disorders, such as schizophrenia (Susser et al., 1995).
In addition to the immediate risks and functional impairments, the psychological distress of experiencing untreated psychotic symptoms can profoundly affect an individual's mental well-being, contributing to conditions like depression and anxiety (Ritsner et al., 2000).
In summary, while Brief Psychotic Disorder is, by nature, short-lived, the repercussions of leaving it untreated can be long-lasting and significantly impairing. The risks of self-harm, functional disruption, and potential progression to more severe mental disorders underscore the importance of timely and effective interventions.
Summary
In light of the extensive insights, Brief Psychotic Disorder is a significant mental health condition characterized by sudden and transient psychotic symptoms. The etiology remains intricate, suggesting the need for further research. However, the disorder's potentially distressing and debilitating nature is precise, with risks of self-harm, disrupted daily functions, and potential progression to more chronic conditions (Rabinowitz et al., 2006; Susser et al., 1995). The intertwining nature of comorbidities complicates diagnosis and underscores the importance of comprehensive assessments. However, amidst these challenges, there is a resounding message of hope.
With appropriate and timely interventions, many individuals experience a full recovery (Wiersma et al., 1998). Moreover, antipsychotic medications, psychotherapy, and family interventions have shown promising outcomes in alleviating symptoms and restoring daily functioning (Wykes et al., 2008; Pharoah et al., 2010). It is essential, though, for individuals and their families to remain vigilant.
Monitoring for signs of recurrence is critical since Brief Psychotic Disorder can re-emerge. In doing so, early detection and intervention can minimize potential complications. In a broader sense, the psychological community's advancements in understanding and managing Brief Psychotic Disorder offer renewed hope for affected individuals and highlight the significance of continued research and nuanced care in promoting mental well-being.
References
Arndt, S., Tyrrell, G., Flaum, M., & Andreasen, N. C. (1991). Comorbidity of substance abuse and schizophrenia: The role of pre-morbid adjustment. Psychological Medicine, 21(2), 379-388.
Baldwin, D. S., Anderson, I. M., Nutt, D. J., Allgulander, C., Bandelow, B., den Boer, J. A., ... & Malizia, A. (2005). "Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology." Journal of Psychopharmacology, 29(5), 403-439.
Bhugra, D., & Bhui, K. (2000). Transcultural psychiatry: Epidemiology, assessment, and treatment. Psychiatric Clinics, 23(3), 545-567.
Brockington, I. (2004). Postpartum psychiatric disorders. The Lancet, 363(9405), 303-310.
Caton, C. L. M., Shrout, P. E., Eagle, P. F., Opler, L. A., Felix, A., & Dominguez, B. (2005). "Risk factors for homelessness among women with schizophrenia." American Journal of Public Health, 95(2), 250-255.
Dixon, L. (1999). Dual diagnosis of substance abuse in schizophrenia: Prevalence and impact on outcomes. Schizophrenia Research, 35(Suppl), S93-S100.
Hanzawa, S., Bae, J. K., Bae, Y. J., Chae, M. H., & Tanaka, H. (2011). Psychological impact on caregivers traumatized by the violent behavior of a family member with schizophrenia. Asian Journal of Psychiatry, 4(2), 127-131.
Howes, O. D., & Kapur, S. (2009). The dopamine hypothesis of schizophrenia: Version III—The final common pathway. Schizophrenia Bulletin, 35(3), 549-562.
Kelleher, I., & Cannon, M. (2011). Psychotic-like experiences in the general population: Characterizing a high-risk group for psychosis. Psychological Medicine, 41(1), 1-6.
Kendler, K. S., Karkowski, L. M., & Walsh, D. (1998). The structure of psychosis: Latent class analysis of probands from the Roscommon Family Study. Archives of General Psychiatry, 55(6), 492-499.
Keshavan, M. S., Haas, G., Miewald, J., Montrose, D. M., Reddy, R., Schooler, N. R., & Sweeney, J. A. (2003). Prolonged untreated illness duration from prodromal onset predicts outcome in first episode psychoses. Schizophrenia Bulletin, 29(4), 757-769.
Kessing, L. V. (1999). Severity of depressive episodes according to ICD-10: Prediction of risk of relapse and suicide. The British Journal of Psychiatry, 174(4), 353-356.
Maj, M. (2007). "Psychiatric comorbidity: An artefact of current diagnostic systems?" The British Journal of Psychiatry, 190(4), 299-304.
Malla, A., Norman, R., & Joober, R. (2005). First-episode psychosis, early intervention, and outcome: What have we learned? Canadian Journal of Psychiatry, 50(14), 881-891.
Marder, S. R., Davis, J. M., & Chouinard, G. (1997). The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: Combined results of the North American trials. The Journal of Clinical Psychiatry, 58(12), 538-546.
Melle, I., Johannesen, J. O., Friis, S., Haahr, U., Joa, I., Larsen, T. K., ... & Rund, B. R. (2004). Early detection of the first episode of schizophrenia and suicidal behavior. The American Journal of Psychiatry, 161(5), 820-826.
Mendez, M. F., Shapira, J. S., & McMurtray, A. (2008). Acute paranoid symptoms due to sleep deprivation. The American Journal of Psychiatry, 165(6), 778.
Mojtabai, R. (2006). Psychotic-like experiences and interpersonal violence in the general population. Social Psychiatry and Psychiatric Epidemiology, 41(3), 183-190.
Monroe, S. M., & Simons, A. D. (1991). Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin, 110(3), 406-425. This reference provides broader insight into the role of stress in triggering psychological disorders.
Myers, D. H., Davies-Jones, C., Chitkara, R., Jackson, M. A., & Glover, V. (1991). Psychotic reaction to childbirth. The British Journal of Psychiatry, 158(2), 238-241.
Myin-Germeys, I., & van Os, J. (2007). Stress-reactivity in psychosis: Evidence for an affective pathway to psychosis. Clinical Psychology Review, 27(4), 409-424.
Perry, Y., Taylor, M., & Shaw, B. (2007). "You're just gonna waste a good brain": Perceptions of psychosis by young people at risk. Australian and New Zealand Journal of Psychiatry, 41(10), 834-838.
Pharoah, F., Mari, J., Rathbone, J., & Wong, W. (2010). Family intervention for schizophrenia. Cochrane Database of Systematic Reviews, (12).
Rabinowitz, J., Levine, S. Z., Häfner, H., & Rabinowitz, J. (2006). A population based elaboration of the role of age of onset on the course of schizophrenia. Schizophrenia Research, 88(1-3), 96-101.
Ran, M. S., Mao, W. J., Chan, C. L., Chen, E. Y., & Conwell, Y. (2015). Gender differences in outcomes of acute and transient psychotic disorders: A 6-year incidence study in Hong Kong. Australian & New Zealand Journal of Psychiatry, 49(4), 377-385.
Riordan, D., Rylance, G., & Berry, C. (1996). Psychosis, physical aggression towards others and HIV disease. The British Journal of Psychiatry, 168(6), 680-685.
Ritsner, M. S., Modai, I., & Endicott, J. (2000). Differences in quality of life domains and psychopathologic and psychosocial factors in psychiatric patients. The Journal of Clinical Psychiatry, 61(11), 880-889.
Salvatore, P., Baldessarini, R. J., Tohen, M., Khalsa, H. M., Sanchez-Toledo, J. P., Zarate Jr, C. A., ... & Maggini, C. (2007). McLean-Harvard International First-Episode Project: Two-year stability of DSM-IV diagnoses in 500 first-episode psychotic disorder patients. Journal of Clinical Psychiatry, 68(2), 210-216.
Spiegel, D., Loewenstein, R. J., Lewis-Fernández, R., Sar, V., Simeon, D., Vermetten, E., ... & Dell, P. F. (2011). Dissociative disorders in DSM-5. Depression and anxiety, 28(9), E17-E45.
Susser, E., Wanderling, J., & Lavelle, J. (1994). Epidemiology of nonaffective acute remitting psychosis vs schizophrenia. Sex and sociocultural setting. Archives of General Psychiatry, 51(4), 294-301.
Susser, E., Wanderling, J., & Lavelle, J. (1995). Acute transient psychotic disorders and subsequent schizophrenia in a developing country. The British Journal of Psychiatry, 167(6), 686-692.
Thirthalli, J., & Benegal, V. (2006). Psychosis among substance users. Current Opinion in Psychiatry, 19(3), 239-245.
Tollefson, G. D., Beasley, C. M. Jr, Tran, P. V., Street, J. S., Krueger, J. A., Tamura, R. N., ... & Breier, A. (1997). Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform disorders: Results of an international collaborative trial. The American Journal of Psychiatry, 154(4), 457-465.
Wiersma, D., Nienhuis, F. J., Slooff, C. J., & Giel, R. (1998). Natural course of schizophrenic disorders: A 15-year follow-up of a Dutch incidence cohort. Schizophrenia Bulletin, 24(1), 75-85.
Wykes, T., Steel, C., Everitt, B., & Tarrier, N. (2008). Cognitive behavior therapy for schizophrenia: Effect sizes, clinical models, and methodological rigor. Schizophrenia Bulletin, 34(3), 523-537.